A Nanometer Resolution Wearable Wireless Medical Device for Non Invasive Intracranial Pressure Monitoring
A brain injury, stroke, or other medical condition can cause increased intracranial pressure (ICP) inside the skull. Intracranial hypertension is a serious medical problem that can cause severe brain or spinal cord impairments and even be life-threatening.
Traditionally, medical practitioners have used direct intracranial pressure (ICP) monitoring procedures to assess ICP and compliance. However, these methods involve surgical or other invasive procedures and are associated with numerous complications. The number of cases of intracranial hemorrhages, infections, and lesions after direct ICP is significant enough to look for other alternatives.
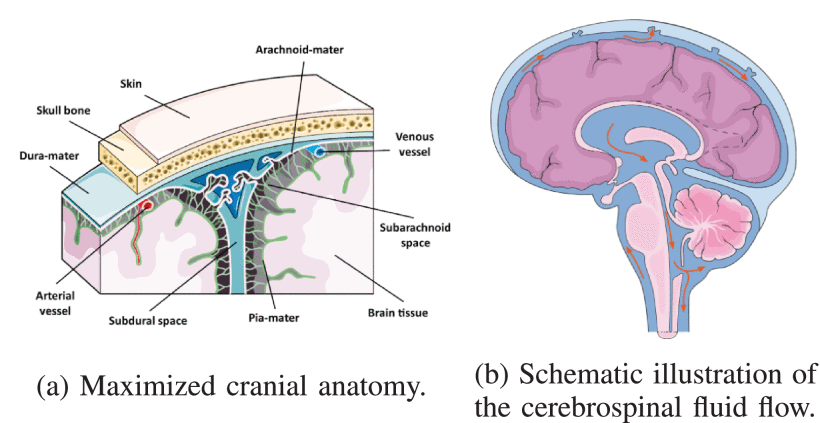
Researchers have extensively studied a few Non-invasive intraocular pressure (NIICP) monitoring techniques based on optic nerve sheath diameter, intraocular pressure, ophthalmo-dynamometry, and ophthalmic blood flow. Recent technological advancements in sensors and nanofabrication have allowed researchers to study bone limitations. The human skull is deformable and can be used as a physical parameter to detect changes in intracranial volume and pressure.
The researchers present the design, development, and evaluation of a non-invasive, wireless sensor for ICP by sensing and measuring skull deformation. They measured the deformation in the parietal region of a human skull using strain gauges as sensors in a laboratory setting. A balloon was inflated inside the head skull to simulate ICP variations. The experiment showed an almost linear correlation between ICP variations and skull deformation.
The proposed device mainly comprises a mechanical transducer that captures the nanometric displacements of the skull and a high-resolution, high-speed analog-to-digital converter. A cantilever beam, strain gauges, and a sensor pin are embedded in an enclosed support, enabling a wearable format on a headband.
The device is fixed on the head such that the cantilever beam is in the frontotemporal region, with the sensor pin touching the scalp. The cardiac pumping dilates the intracranial arteries, causing variations in intracranial volume and pressure. The increased ICP can cause nanometric skull bone deformation. The deformation in the skull displaces the sensor pin, causing a mechanical deformation. This mechanical deformation is measured and transduced by strain gauges.
The analog signal is converted to digital and sent to a cloud-based processor via the internet for further analysis and reporting. The report comprises the ICP waveform signal over time and a pulse morphology expressed as the average per minute.
The study evaluated the sensor prototype for the stability of the measurements, nanometric sensitivity, and waveform parameter reproduction. The NIICP signal has a typical amplitude of 5 μms and requires a resolution of at least 1% of this amplitude for a NIICP pulse morphology analysis. A nanometre-shift test system demonstrated a sensor resolution of 40 nm. It responds dynamically to NIICP signals from 50 to 180 bpm without significant distortion.
The NIICP monitoring system demonstrates excellent accuracy, measurement stability, sensitivity, and reproduction of ICP pulse morphology parameters, with good signal pickup and little data loss. The prototype has the potential as a low-risk, portable device to provide real-time and consistent ICP pulse waveform for clinical analysis and interpretation.